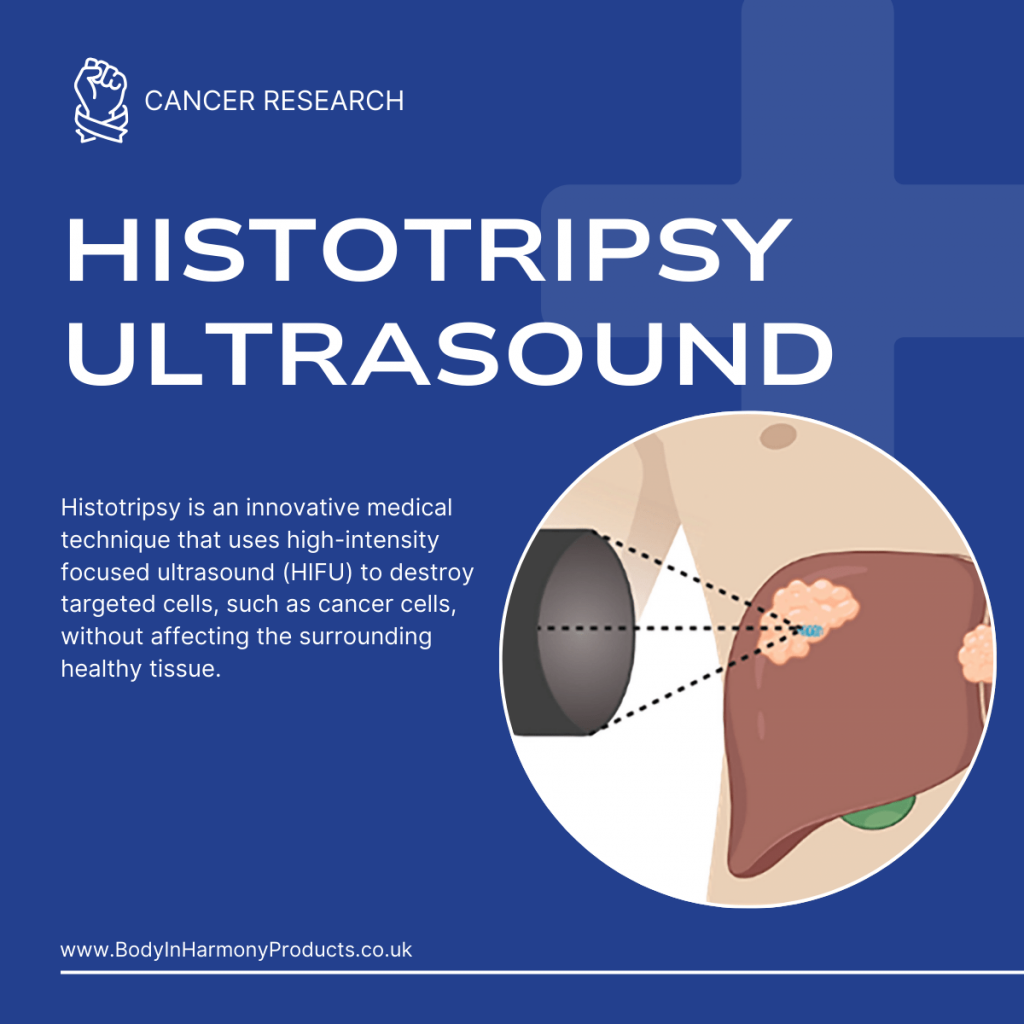
What is Histotripsy?
Histotripsy is an innovative medical technique that uses high-intensity focused ultrasound (HIFU) to destroy targeted cells, such as cancer cells, without affecting the surrounding healthy tissue. By delivering precise bursts of acoustic energy, the procedure generates microbubbles that collapse and induce mechanical disruption of cellular structures. This non-invasive method is gaining attention as a promising alternative to conventional cancer treatments like chemotherapy, radiation, and surgery.
The Emergence of Histotripsy
Initially developed as a tool for non-invasive surgical procedures, histotripsy has evolved into a potential game-changer in oncology. Researchers have been investigating its efficacy in eliminating tumours while preserving organ function. With recent advancements in imaging and acoustic technologies, histotripsy has become increasingly precise, opening new doors for targeted cancer therapy.
Histotripsy works by creating a highly localized mechanical effect within the tumours. Ultrasound waves are focused on a specific area, causing cavitation—the rapid formation and collapse of microbubbles. This process disrupts cellular membranes and organelles, ultimately leading to cell death. Unlike thermal ablation, which relies on heat to destroy tissue, histotripsy utilises mechanical forces, minimizing the risk of collateral damage.
Comparison to Traditional Cancer Treatments
Traditional cancer treatments often involve systemic approaches, such as chemotherapy, which can harm healthy cells and cause significant side effects. Radiation therapy, while effective, may also lead to long-term damage to surrounding tissues. In contrast, histotripsy offers a localised, non-invasive solution with fewer risks. It allows clinicians to target tumours with pinpoint accuracy, potentially improving outcomes and reducing recovery times.
Scientific Evidence Supporting Histotripsy
- Laboratory Studies
Preclinical studies have demonstrated the efficacy of histotripsy in selectively destroying cancer cells. In vitro experiments on various cancer cell lines, including breast, liver, and pancreatic cancer, have shown significant tumour reduction following exposure to focused ultrasound. For instance, a 2020 study published in Scientific Reports highlighted how histotripsy effectively disrupted tumour cells without damaging adjacent healthy tissue.
- Clinical Trials
Recent clinical trials have begun to validate the safety and effectiveness of histotripsy in human patients. A pilot study conducted in 2022 involved patients with early-stage liver cancer and reported tumour shrinkage in over 85% of cases. Additionally, participants experienced minimal side effects compared to those undergoing conventional treatments. These findings underscore the potential of histotripsy as a viable cancer therapy.
The Benefits of Histotripsy
Minimally Invasive Approach
Unlike traditional surgical procedures, histotripsy does not require incisions or physical contact with the tumour. This non-invasive technique reduces the risk of infection and promotes faster recovery.
Enhanced Precision
Advanced imaging technologies, such as MRI and ultrasound, guide the application of focused ultrasound waves, ensuring that only the targeted tumour cells are affected. This precision reduces the likelihood of harming surrounding tissues.
Reduced Side Effects
Histotripsy’s mechanical approach eliminates the need for systemic drugs or radiation, significantly lowering the risk of common side effects like nausea, fatigue, and organ toxicity.
Future Directions and Applications
Beyond Oncology
While histotripsy has shown immense promise in cancer treatment, its applications extend to other medical fields. Researchers are exploring its use in breaking down kidney stones, treating cardiovascular conditions, and even delivering drugs directly to targeted tissues.
Integration with Other Therapies
Histotripsy could be combined with existing therapies to enhance treatment efficacy. For example, pairing it with immunotherapy may boost the immune system’s ability to fight residual cancer cells, creating a synergistic effect.
Conclusion
Histotripsy represents a breakthrough in cancer treatment, offering a precise, minimally invasive, and effective method for destroying tumour cells. Laboratory studies and early clinical trials have provided compelling evidence of its potential, highlighting its advantages over traditional approaches.
As research continues, histotripsy could transform the landscape of oncology and other medical disciplines. By prioritising precision and patient safety, it has the potential to revolutionise how we approach complex diseases, offering hope to millions worldwide.
As research continues, histotripsy could transform the landscape of oncology and other medical disciplines. By prioritising precision and patient safety, it has the potential to revolutionise how we approach complex diseases, offering hope to millions worldwide.